Review: “Aspirin responsive platelet thrombophilia in essential thrombocythemia and polycythemia vera,” by Jan Jacques Michiels, et al., World Journal of Hematology, May 6, 2013, doi:10.5315/wjh.v2.i2.20
This sprawling, carefully annotated study of the role of aspirin-responsive  thrombophilia (coagulability) in ET and PV is a comprehensive and sometimes daunting review of cellular and vascular impacts of essential thrombocythemia and polycythemia vera and the means to assess and modify the risk of hemorrhage and thrombosis.
thrombophilia (coagulability) in ET and PV is a comprehensive and sometimes daunting review of cellular and vascular impacts of essential thrombocythemia and polycythemia vera and the means to assess and modify the risk of hemorrhage and thrombosis.
Its 24 pages, illustrated with slides, tables, and figures painstakingly describe the molecular and hematological effects of ET and PV and biologic pathways involved in reducing erythromelalgia (pain, inflammation) and risk of vascular or cardiac events. Our review focuses narrowly on the impact of aspirin in reducing both thrombotic complications and erythromelalgia although the paper itself , as indicated by the Michiels’ outline, goes much further afield in near encyclopedic review of therapeutic options, lavishly footnoted.
PAPER OUTLINE
Abstract and Introduction
Histopathology of erythromelalgia in thrombocythemia
Involvement of platelets as the cause of erythromelalgia in ET
Migraine-like microvascular cerebral ischemic attacks in ET
Activated platelets, leukocytes and endothelial cells in ET and PV
Thrombotic and hemorrhagic risk stratification in ET
Thrombohemorrhagic ET risk and the need to reduce platelet count without leukemogenic agents
Thrombosis and hemorrhage in thrombocythemia related to von Willebrand factor.
The role of hematocrit and platelets in thrombosis risk.
Assessment in PV: Reversal by phlebotomy and low dose aspirin
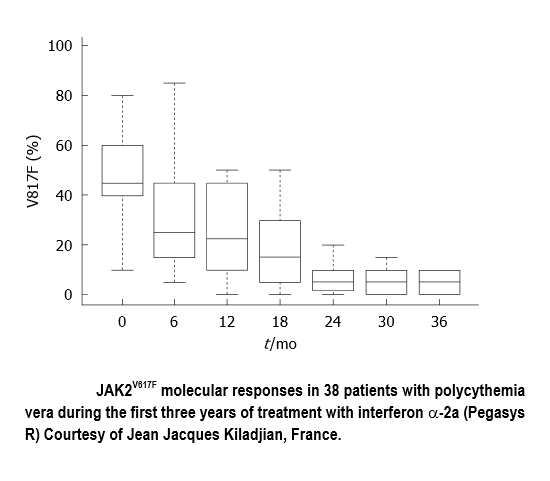
Induction of complete hematological remission by IFN in early PF and ET
Molecular etiology of platelet mediated arteriolar thrombosis in ET and PV
“Erythromelalgia is the main pathognomonic and presenting symptom in patients with essential thrombocythemia and thrombocythemia associated with polycythemia vera.”
Michiels immediately focuses on the painful swelling and burning frequently affecting extremities of patients with chronic MPNs. The condition described in 1878 by Silas Weir Mitchell, who supplied a manuscript footnote tracing the etymological roots of the condition i.e., The “burning painful and red congestion of the foot and hand disorder might conveniently be labeled erythromelalgia, (From the Greek: erthyros=red, melos=extremity and algos=pain.)”
At the time the condition, then called Mitchell’s Disease, was not separated into the more common form of erythromelalgia that arises from a disease state and primary or congenital idiopathic erythromelalgia.
L.A. Smith in the American Heart Journal (1938) first described aspirin’s effect in promptly relieving erythromelalgic pain over a period of approximately three days. Michiels established the involvement of platelets’ role in erythromelalgia through evidence of platelet consumption, platelet proliferation and increased platelet activation markers obtained through skin biopsy of swollen red areas. It was Michiels and his associates who. during the 1975-1981 period, discovered “the specific subset of patients with burning painful red extremities, who experienced clinical relief with aspirin, all had elevated platelet counts associated with thrombocythemia…or associated with polycythemia vera.”
Thrombophilia, a state of hypercoagulability, is a blood coagulation abnormality that increases the risk of thrombosis or blood clots in blood vessels. A core contention of this paper and an earlier Michiels publication (2002) is his observation: “Complete relief of erthyromelalagic …pain is obtained with the cyclooxygenase inhibitor aspirin…” (Cyclooxygenase (COX) is an enzyme that is responsible for the formation of prostanoids. The three main groups of prostanoids — prostaglandins, prostacyclins, and thromboxanes — are each involved in the inflammatory response.)
“Aspirin sensitive erythromelalgia is characterized by warm, red, congested extremities and painful burning sensations and causally linked to thrombcythemia in various myeloproliferative disorders….
“Acroparaesthesias (tingling, numbness, stiffness) “usually preceed the disabling red, swollen burning distress. Warmth intensifies the discomfort and cold provides relief …The long lasting effect of a single dose of aspirin is so specific for erythromelalgia that it can be used as a diagnostic criterion.”
Although he couldn’t contribute patients to the European Collaboration on Low Dose Aspirin in PV (ECLAP) “because nearly all PV patients in…The Netherlands were on low dose aspirin,” Michiels could call on ECLAP data to support his contention that aspirin control of platelet function—coupled with normalizing platelet levels through use of platelet lowering agents “are effective in the prevention of platelet- mediated microvascular circulatory disturbances in thrombocythemia vera.
THE COX-1 inhibition effect.
Two Forms of Cyclooxygenase (COX)
In the 1990s, researchers discovered that two different COX enzymes existed, now known as COX-1 and COX-2. Cyclooxygenase-1 (COX-1) is present in most tissues. In the gastrointestinal tract, COX-1 helps in maintaining the stomach lining and is also critically involved in platelet and kidney function. Cyclooxygenase-2 (COX-2) is found largely at inflammation sites. COX-1 and COX-2 convert arachidonic acid to prostaglandin, resulting in pain and inflammation. Their biological functions make indiscriminate inhibition of COX-1 undesirable while COX-2 is targeted for inhibition.
“Clinicians .” conclude Michiels, “will be reluctant to postpone the use of hydroxyurea in early stage PV as long as it is a conservative approach using phlebotomy aiming at a hematocrit below 0.45, on top of low dose aspirin for the control platelet function, and if indicated, anagrelide for the control of platelet[ levels.]”.

© MPN Quarterly Journal, 2013. This work is licensed under a Creative Commons Attribution-NonCommercial No-Derivs 3.0 Unported License.